SUMMARY: Every healthcare leader knows the feeling: the schedule looks fine, the staffing plan looks reasonable, the budget assumptions look sound and yet things still don’t line up in practice. Coverage scrambles keep happening. External spend creeps upward. New providers take too long to get deployed. Burnout flares up in unexpected places. This post explains why alignment slips, why it’s so hard to rebuild once it does, and what high-performing organizations do to restore a shared operational truth.
It’s tempting to attribute drift issues to isolated problems: a tough month, a surge in demand, a communication hiccup. But most organizations aren’t dealing with isolated issues at all. They’re dealing with an alignment problem.
Alignment breaks down quietly, not dramatically. It’s rarely the result of a single failure. Instead, it’s a slow divergence. It's often brought on by different teams interpreting the same workforce reality in different ways, guided by different timelines, metrics, and operational pressures. By the time the effects become visible, the drift has already done its damage.
1. Drift Begins When Teams Aren’t Working From the Same Staffing Story
Most staffing decisions are shaped by perspective, not intent.
- Finance looks at the year.
- Operations looks at the week.
- Scheduling looks at the next 6–12 hours.
- Clinical leaders look at the wellbeing of their teams.
- Credentialing looks at the process, not the pace of operations.
- Recruiting looks at long-term supply.
Everyone is acting rationally within their responsibilities but the perspectives aren’t aligned. This is how misalignment begins: not through disagreement, but through distance. When the story of “what’s happening with staffing” differs from group to group, every decision (even well-intentioned ones) nudges the organization in a slightly different direction.
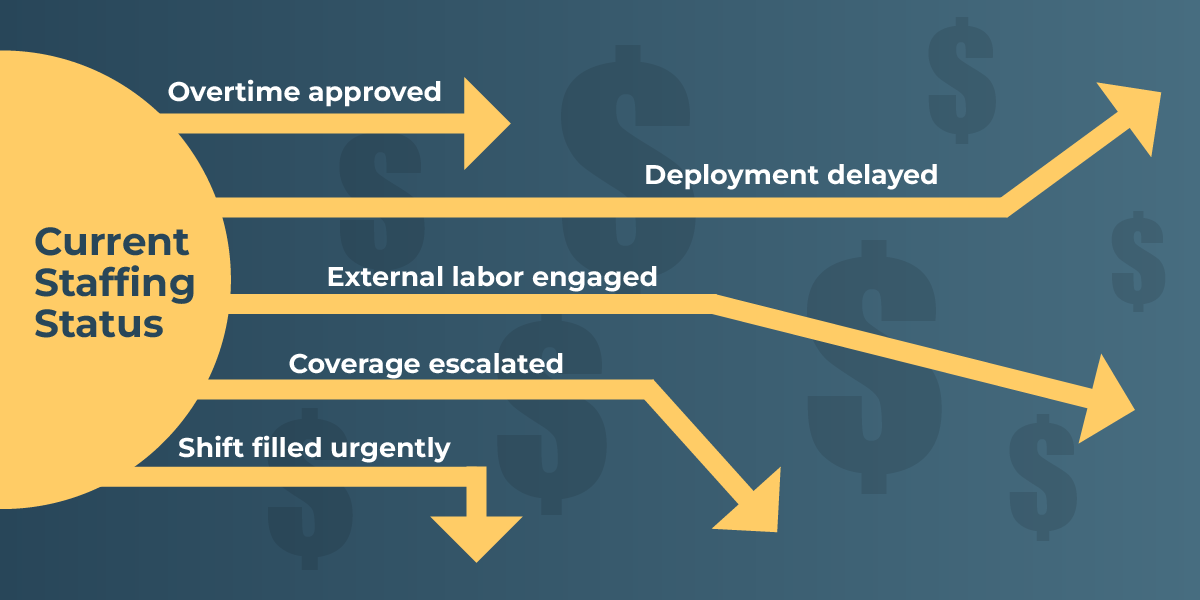
2. Minor Disconnects Compound Into Meaningful Operational & Financial Impact
Workforce misalignment rarely appears as a dramatic event. It typically emerges from small, almost forgettable moments:
- A provider’s availability changes, but only one team sees it.
- Credentialing approves someone, but the update hits someone’s inbox at the wrong time.
- Scheduling fills a shift because the gap is urgent, not realizing internal capacity was only a day away from being ready.
- A site gets busier, but demand data isn’t shared broadly enough to adjust schedules in time.
- A new hire becomes fully eligible, but template updates lag behind.
None of these incidents feel consequential on their own. But the compounding effect is real and costly. Organizations start relying on external labor not because they lack internal supply, but because internal information doesn’t surface quickly enough to guide decisions.
This is the quiet, operational version of drift: nothing is broken, but nothing aligns.
3. Fragmented Systems Turn Staff Planning Into Guesswork
Even well-coordinated teams struggle when their tools don’t work together.
Most organizations rely on a patchwork of systems:
- Onboarding
- Credentialing
- Scheduling
- HRIS
- Agency systems
- Spreadsheets
- Inboxes
- Finance reporting tools
Each system is accurate in its own way, but none reflect the whole staffing reality. This fragmentation forces teams to rely on assumptions, tribal knowledge, and manual triage, not real-time truth.
When your view of the workforce depends on which system you’re looking at, alignment becomes impossible to sustain.
4. When Alignment Fails, the Consequences Spread Quickly
Operational misalignment is expensive — not only financially, but organizationally.
Operational consequences
- Recurring coverage scrambles
- Slower response to changes in demand
- Onboarding-to-scheduling delays
- Lack of predictable staffing rhythms
Financial consequences
- Reliance on external labor by default
- Overtime driven by workload imbalance
- Unforeseen premium shifts
- Budgets that drift away from original assumptions
Clinical consequences
- Uneven workload distribution
- Rising frustration among providers
- Avoidable burnout risk
Leadership consequences
- No one is fully confident the staffing plan reflects reality
- Performance initiatives stall because the inputs aren’t aligned
Organizations often try to fix these problems tactically, but the root issue is strategic: teams don’t share a single understanding of the workforce.
5. High-Performing Organizations Restore Alignment Through Shared Visibility
Alignment doesn’t come from more meetings, more messaging, or more policies. It comes from a shared understanding of staffing truth. High-performing organizations focus on three core practices:
A. One unified workforce picture
Instead of asking teams to reconcile their systems, they create a single view that connects:
- Readiness
- Eligibility
- Internal availability
- Scheduling
- External usage
- Workload balance
- Cost impact
This removes ambiguity. When the data is unified, so are the decisions.
B. Short, consistent operational rhythms
Weekly or twice-weekly touchpoints keep Finance, Operations, Scheduling, Clinical Leadership, and Credentialing on the same page — not to rehash problems, but to ensure the assumptions guiding decisions are aligned.
C. Internal capacity becomes the starting point, not the afterthought
When internal options are easy to see, internal options get used. This reduces avoidable external spend and stabilizes operations.
Alignment isn’t about agreement. It’s about clarity.
6. What Re-Alignment Looks Like in Practice
When alignment is restored, leaders can feel the difference:
- Staffing decisions become calmer and more predictable
- New providers get deployed quickly
- External spend drops because internal supply is visible
- Budgets match operational reality
- Workload becomes more balanced across teams
- Leaders stop “discovering” issues late — they see them before they escalate
- Teams trust the same numbers, instead of maintaining their own versions
The result is operational stability. Not because the work is easier, but because the truth is shared.
How Kimedics Helps Organizations Rebuild Alignment
Kimedics gives healthcare organizations the visibility and connected workflows needed to maintain workforce alignment, even in complex and fast-moving environments.
Kimedics provides:
- A single source of staffing truth across internal and external resources
- Real-time visibility into readiness, availability, and utilization
- Workflows that connect credentialing, scheduling, and deployment
- Clarity around internal capacity before external options are used
- Cost transparency that finance can rely on
- Operational rhythms teams can anchor around
- Insights that prevent avoidable drift and overspend
Alignment becomes achievable and sustainable when teams can finally see the same reality.
Ready to bring your workforce teams back into alignment?
Request a Demo
Learn more about Kimedics
Kimedics is a provider utilization management platform. We help healthcare organizations gain visibility across internal and external staffing to reduce complexity and improve financial performance. For more information, book a demo or email kimedics@kimedics.com