Friday the 13th has a way of surfacing uncomfortable stories. This one is real.
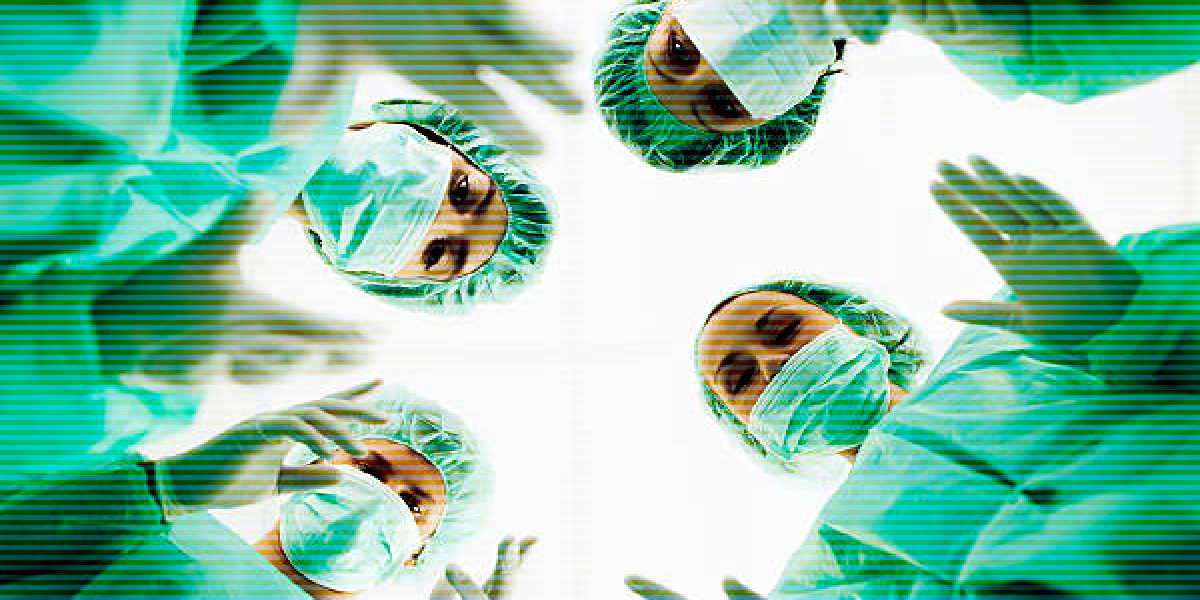
In 2023, at a hospital in the UK, a consultant anesthetist left a patient under general anesthesia in the middle of a surgical procedure. The departure was unplanned. The operating room was active. The patient was fully dependent on continuous clinical coverage.
The anesthetist returned several minutes later. The patient was not harmed. The incident was later reviewed by a medical tribunal and classified as serious misconduct.
It’s an extreme case. It’s also a useful one. Not because it reflects typical clinician behavior, but because it exposes how fragile clinical operations can become when coverage assumptions go unexamined.
The uncomfortable truth
Most healthcare organizations design schedules around presence, not resilience.
We assume:
- The scheduled clinician will be available
- Coverage equals safety
- Edge cases are rare enough to handle reactively
But when a single clinician’s absence, planned or unplanned, can put a patient at risk, that’s not a behavioral issue. It’s an operational one. The UK case is shocking because it’s dramatic. More often, the failure mode is quieter:
- A specialist stretched across too many cases
- A call schedule built around the same dependable names
- A department where only one or two clinicians can cover a critical role
Nothing breaks. Until it does.
Single points of failure
In many hospitals, there are clinicians who quietly become linchpins:
- The only provider credentialed for a complex procedure
- The person everyone calls when the schedule falls apart
- The clinician who “always says yes”
Over time, reliance escalates. Workload concentrates. Burnout risk increases.
From the outside, the schedule still looks covered. From the inside, the margin for error is gone.
When something unexpected happens (illness, exhaustion, refusal, or a breaking point), the system has no buffer.
This isn’t about blame
It’s tempting to focus on individual conduct in stories like this. That misses the point.
Operational risk rarely announces itself as risk. It shows up as:
- Increasing exceptions
- Quiet overuse of a few clinicians
- Last-minute fixes that slowly become standard practice
By the time leadership notices, options are limited, expensive, or both. The real question isn’t “How could this happen?” It’s “Would we see our own version of this coming?”
The Friday the 13th question
If a critical clinician in your organization became unavailable at the worst possible moment, what would actually happen?
Not the policy answer. The real one. That gap (between what we assume and what we can prove) is where staffing risk lives.
Extreme cases get attention because they’re rare. Operational failures persist because they’re familiar.
Most staffing breakdowns don’t look like crises when they begin. They look like reasonable workarounds, trusted clinicians stepping up, and schedules that technically “work.” Over time, those choices narrow the margin for error until a single absence becomes a system-level risk.
The question isn’t whether a worst-case scenario will ever happen. It’s whether you’d recognize the warning signs early enough to prevent it.
Reader poll
When a single critical clinician becomes unavailable at the worst possible moment, where do you turn?
- I’d utilize a float pool
- I would pay premium to bring in another clinician
- I'd pay overtime for a scheduled clinician to cover
- I would cancel the procedure or visit
- Hope & pray
Click here to complete this quick anonymous poll or see others' answers.