The Workforce Misdirection Series: How Healthcare Teams Lose Their Way and How to Get Back on Course (5 of 6)
SUMMARY: Most healthcare leaders believe they have a solid sense of provider utilization. They review productivity reports, track hours, understand clinic schedules, and monitor payroll. On paper, everything appears accounted for.
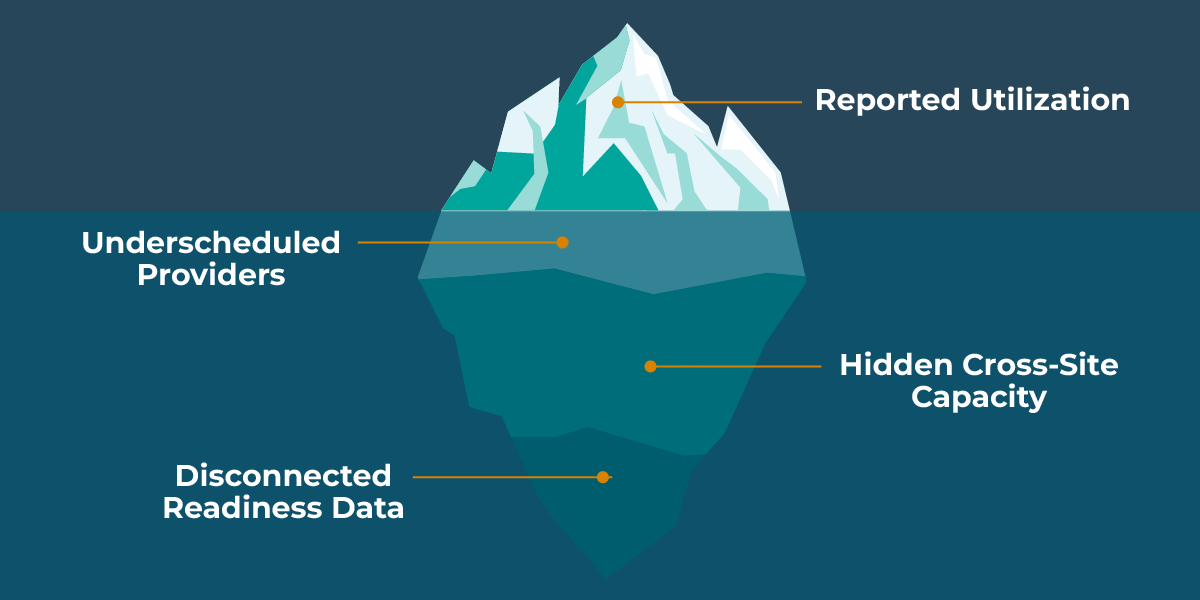
But in nearly every organization, there is a wide gap between reported utilization and true provider deployment. The data gives the impression of full capacity while real internal supply sits dormant, misallocated, or invisible. This is the utilization mirage: a system that makes leaders believe their workforce is fully used when, in reality, significant internal opportunity goes untapped.
This post explains how the mirage forms, why it persists, and how organizations can finally see (and use) their real internal capacity.
1. Utilization Is Measured in Fragmented, Incomplete Ways
Most utilization reporting focuses on one or two data sources:
- Clinic schedules
- Timesheets
- RVUs or productivity systems
- Payroll hours
Each dataset shows a piece of the picture but not the whole thing. What’s missing?
- Cross-location availability
- Providers who could work but aren’t scheduled
- Providers ready for deployment but not added to templates
- Under-the-radar internal capacity
- Tasks performed outside EHR workflows
- Urgent coverage providers routinely absorb
When the underlying data is incomplete, even the cleanest dashboards produce distorted conclusions.
2. “Fully Scheduled” Doesn’t Mean “Fully Utilized”
Leaders often assume:
- “The schedule is full, so providers must be fully deployed.”
- “If they were available, they’d be scheduled.”
- “If we needed internal coverage, someone would raise it.”
But in practice:
- A provider can appear “full” while carrying mostly low-acuity or unevenly distributed shifts.
- A provider can be internally available but hidden behind outdated preference data.
- Newly onboarded clinicians can be ready to work but still absent from scheduling templates.
- Providers with flexible capacity often aren’t flagged in time to prevent external spend.
The data gives an illusion of full deployment. The reality is much looser.
3. Invisible Underscheduling Is One of Healthcare’s Most Expensive Problems
Underscheduling rarely triggers alarms because:
- Providers don’t complain — they assume it will get fixed.
- Finance sees only payroll, not potential.
- Operations teams assume the data is current.
- Clinical leaders aren’t always looped into scheduling inefficiencies.
- Agencies provide quick fixes that mask internal gaps.
The result?
- Internal resources go unused.
- External spend grows to fill “gaps” that shouldn’t exist.
- Some providers become overloaded while others wait for work.
- Organizations believe they need to hire when they actually need clarity.
The mirage creates waste that looks like necessity.
4. Eligibility, Credentialing, and Onboarding Gaps Distort Utilization
One of the biggest causes of false utilization is misalignment between:
- Readiness
- Availability
- Eligibility
- Scheduling templates
A clinician may be:
- Fully credentialed
- Ready for multiple sites
- Available to work
…but still not visible to schedulers because:
- Credentialing clearance wasn’t communicated.
- Their site eligibility wasn’t updated.
- Their availability wasn’t entered into the right system.
- Their profile wasn’t added to the schedule.
- Their cross-credentialing status is buried in emails.
This creates the illusion of scarcity, even when the organization has available internal supply.
5. Leaders Don’t See Utilization Drift in Real Time
Utilization issues rarely announce themselves. They build slowly:
- A few missed internal coverage opportunities
- A growing reliance on agencies
- A handful of providers becoming overextended
- A handful becoming underused
- A new clinician ready to work but not yet plugged in
- A provider’s preferences changing without being captured
By the time the quarterly or annual data catches up, the drift is already embedded in the system.
This is why leaders feel they’re always solving last month’s problems.
6. Finally Seeing the Real Picture
Organizations that overcome the utilization mirage do one thing differently:
- They analyze utilization across internal, external, and readiness data at the same time.
This lets leaders see:
- Who is overextended
- Who is underutilized
- Who is internally available but unused
- Where cross-site capacity exists
- Where external spend is substituting for internal supply
- Which workflow gaps create false shortages
When you can see true internal supply, decisions change immediately.
- “What gaps do we need agencies for?” becomes “What gaps can we fill internally?”
- “What’s our hiring need?” becomes “Do we need clearer deployment before we hire?”
- “What did we spend?” becomes “What could we have avoided spending?”
The mirage disappears. The strategy becomes clearer.
How Kimedics Helps
Kimedics helps organizations replace the utilization mirage with real visibility across internal capacity, external use, readiness, and deployment. With Kimedics, leaders can:
- See true internal availability
- Identify underused providers
- Compare internal and external coverage side by side
- Detect utilization drift early
- Connect scheduling, readiness, and agency data
- Reduce unnecessary external spend
- Improve workload balance and stability
When leaders finally see the real picture, they make better decisions and spend money where it matters most.
Want a clearer view of how fully your providers are really being used?
Request a Demo
Learn more about Kimedics
Kimedics is a provider utilization management solution. We help healthcare organizations reduce scheduling complexity. For more information, book a demo or email kimedics@kimedics.com