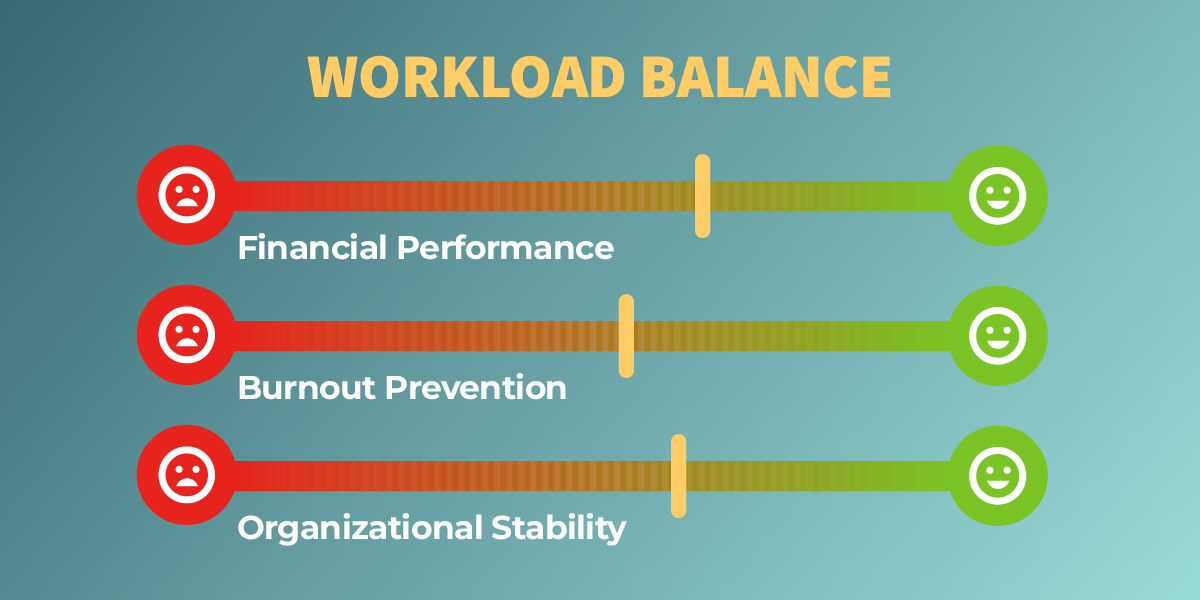
SUMMARY: Healthcare leaders talk often about provider workload, but mostly in terms of fairness, burnout, or morale. Those matter deeply, but they’re only part of the picture. Workload balance is a structural driver of financial performance, clinical stability, and long-term organizational health.
When workloads drift out of balance, the effects ripple through scheduling, spend, provider retention, external reliance, and patient access. Most leaders can sense imbalance when it’s happening. Few can measure it accurately. Even fewer can act on it proactively.
This post explains why workload balance matters more than teams realize, where imbalance comes from, and how organizations can treat workload as a strategic lever rather than a reactive problem.
1. Workload Is More Than Hours. It’s the Full Mix of Responsibilities
Two providers can each work 40 hours a week and have completely different experiences. One might carry:
- Nights and weekends
- Higher-acuity or complex cases
- A steady stream of urgent add-on requests
- Frequent schedule changes
- Informal leadership or teaching duties
Another might have:
- Predictable clinic blocks
- Fewer call demands
- Lower intensity work
- Protected time
- Advance notice for schedule adjustments
On paper, both are “fully utilized.” In reality, only one is on the path to burnout.
Organizations that evaluate workload by hours alone miss the nuance that actually determines sustainability.
2. Workload Imbalance Shows Up Everywhere — Quietly at First
Workload imbalance typically starts subtly:
- A few high performers are always asked to “help out.”
- Last-minute openings go to the same people over and over.
- Underutilized providers wait for assignments that never come.
- Expectations shift without clear communication.
- A handful of clinicians become the “reliable fix” for recurring problems.
Then the operational symptoms begin:
- Rising overtime
- Growing locum use for avoidable gaps
- Declining morale
- Complaints about unpredictability
- Leadership surprises when someone suddenly resigns
These pressures don’t happen in isolation. They compound.
3. The Consequences Are Operational — and Financial
Workload imbalance affects more than burnout. It disrupts the organization’s financial and operational stability.
A. Higher Turnover and Replacement Costs
The providers taking on the heaviest workloads are often your most capable and most recruitable. When they burn out, they leave quickly and expensively.
B. Increased External Coverage
If a portion of your internal workforce is overextended while another segment is underutilized, scheduling becomes reactive. Gaps get filled externally because internal options appear unavailable.
C. Escalating Costs Hidden in Plain Sight
Imbalance turns into:
- Premium-rate shifts
- Agency dependence
- Last-minute locums
- Avoidable overtime
All of which appear “operationally necessary,” even when they’re downstream effects of uneven workload.
4. Erosion of Trust
When some providers consistently carry the load, trust in the system drops. That makes it harder to implement scheduling changes, create flexible staffing models, or ask for collaboration during crunch periods.
Workload imbalance is one of the quietest (and most expensive) operational risks in healthcare.
4. Why Workload Is So Hard to Measure
Organizations struggle with workload because the data lives in too many places:
- Scheduling
- Call assignments
- Shift types
- Productivity systems
- Case complexity
- External coverage usage
- Clinical leadership knowledge
Most tools reduce workload to simple metrics like “hours” or “shifts.”
Those metrics miss:
- Type of work
- Intensity of work
- Timing of work
- Volume of last-minute changes
- Hidden responsibilities
- Informal leadership roles
- Substitution effects (when internal work prevents external spend)
When workload isn’t measured holistically, teams chase symptoms instead of fixing root causes.
5. Treating Workload Balance as a Strategic Lever
The organizations that manage workload well don’t leave it to chance.
They:
-
Track workload across multiple dimensions
- Not just hours — but nights, weekends, call, shift types, and intensity.
-
Identify outliers early
- Both the overextended and the underused.
-
Connect workload data to staffing and financial decisions
- So leaders see the relationship between imbalance and spend.
-
Bring clinical leadership into the conversation
- Workload decisions can’t be purely operational or purely financial — they have to be clinical, too.
-
Rebalance deliberately...
- ...using clear data and shared expectations.
- Balanced workload leads to:
- Predictable costs
- Stable access
- Better retention
- Less external reliance
- Stronger culture
- It is one of the few levers that creates both financial efficiency and provider sustainability.
How Kimedics Helps
- Track workload beyond hours
- Compare distribution across shifts, sites, and specialties
- Identify imbalances early
- Connect workload to cost, coverage, and utilization
- See where internal capacity can offset external spend
Ready to get a clearer handle on provider workload across your organization?
Request a Demo
Learn more about Kimedics
Kimedics is a provider utilization management solution. We help healthcare organizations reduce scheduling complexity. For more information, book a demo or email kimedics@kimedics.com